The end of TB
Syllabus Covered:
GS Paper II - Health & Social Justice
GS Paper III - Science & Tech
Although many believed in the 1980s that tuberculosis (TB) was on the path to elimination, it made a strong comeback due to multiple factors, especially in the United States — re-emerged with more complexity in the late 20th century due to scientific, social, and political neglect.
Historical Timeline & Early Successes
- Mid-20th century: TB cases had been sharply
declining in the U.S. This success was attributed to:
- Better urban sanitation.
- Development and use of antibiotics like streptomycin.
- Widespread vaccination and public health campaigns.
- Improved housing and nutrition.
- By the 1980s, TB incidence had dropped so low that many believed its elimination was inevitable. TB was no longer seen as a major public health threat in developed countries.
Reversal of Gains: The Comeback of TB (Late 1980s–1990s)
Despite early optimism, the 1980s and 1990s saw a shocking resurgence of TB in the U.S. due to the following key reasons:
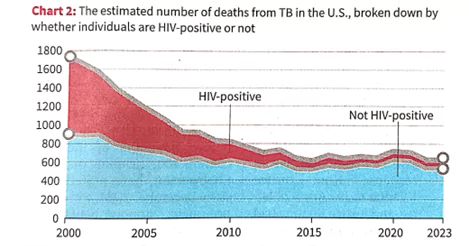
HIV/AIDS Epidemic:
- HIV weakens the immune system, making people highly susceptible to TB infection.
- Co-infection became common, particularly in urban centers.
Funding Cuts:
- In the early 1980s, the U.S. government cut funding for TB control
programs, leading to:
- Neglect in surveillance systems.
- Reduced investment in public health infrastructure.
- Collapse of once-strong tuberculosis clinics and support mechanisms.
Immigration & Urban Vulnerability:
- S. immigration policy changes in the 1960s allowed more people from TB-endemic countries (Africa, Asia, Latin America) to settle.
- Many of these immigrants had latent TB infections, which could later activate, especially under poor living conditions.
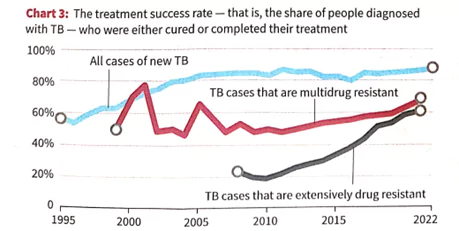
Emergence of Drug-Resistant TB:
- Misuse and incomplete antibiotic treatment led to strains resistant to first-line TB drugs.
- These strains were harder and costlier to treat and more lethal.
Poverty, Overcrowding & Prisons:
- TB outbreaks surged in:
- Homeless shelters.
- Prisons.
- Crowded urban housing.
Between 1985 and 1992, TB cases in the U.S. increased by 20%, reversing decades of progress.
Global Dimensions & WHO Emergency Declaration
- The resurgence wasn’t limited to the U.S.
- Globally, TB was still killing millions, especially in sub-Saharan Africa, South Asia, and parts of Eastern Europe.
- The WHO declared TB a global health emergency in 1993.
- This was due to increasing drug resistance and its synergy with HIV in developing countries.
Scientific and Medical Realities
- Latent TB: Mycobacterium tuberculosis can lie dormant in the body for years, reactivating when immunity drops.
- TB requires long, uninterrupted treatment (6–9 months). Many patients discontinue midway, risking resistance.
- Treating multi-drug-resistant TB (MDR-TB) is costly, time-consuming, and comes with severe side effects.
What Went Wrong?
- The main error was overconfidence.
- By the 1980s, TB was so rare in developed countries that it was de-prioritized in policy and funding.
- Public health experts and doctors warned about possible resurgence, but their voices were largely ignored.
- The system failed to:
- Maintain early detection
- Adapt to new risk groups (HIV patients, immigrants).
- Monitor drug resistance trends in time.
Data and Charts (from the article)
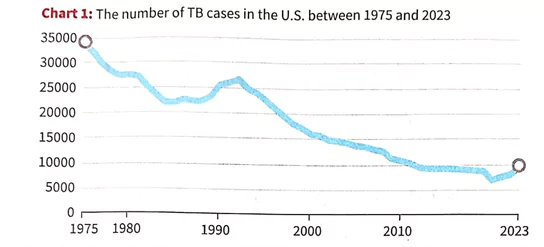
- Charts in the article show:
- A steep drop in TB cases till the early 1980s.
- A spike in the 1990s due to the factors above.
- Correlation between HIV rates and TB incidence.
Lessons for India and the World
- TB is not just a biological disease; it's deeply rooted in poverty, neglect, and systemic failures.
- Elimination requires:
- Consistent funding, even when case numbers are low.
- Community-level surveillance.
- Global cooperation—as migration and travel affect all countries.
- Addressing co-morbidities like HIV, malnutrition, and diabetes.
- Investment in R&D for shorter, safer treatment regimens and better vaccines.
Prelims Questions:
- Which of the following factors contributed to the resurgence of
Tuberculosis (TB) in the United States during the late 1980s and early
1990s?
- The spread of HIV/AIDS
- Emergence of drug-resistant TB strains
- Increased immigration from TB-endemic countries
- Enhanced diagnostic facilities leading to over-reporting
- 1, 2 and 3 only
- 2 and 4 only
- 1, 3 and 4 only
- 1, 2, 3 and 4
- Consider the following statements regarding Tuberculosis (TB):
- TB bacteria can remain dormant in the human body and reactivate later.
- The World Health Organization declared TB a global health emergency in the year 1993.
- TB treatment generally requires a short course of antibiotics lasting about 10-15 days.
- 1 and 2 only
- 2 and 3 only
- 1 and 3 only
- 1, 2, and 3
- The declaration of TB as a “global health
emergency” by WHO was primarily triggered by:
- The development of a highly contagious airborne variant of TB
- Increasing cases of TB among children worldwide
- The emergence of multidrug-resistant TB strains and HIV-TB co-infection
- A pandemic-like global spread of TB within a single year
- “Despite advances in treatment and diagnostics, TB remains a major global health challenge.” In light of this, discuss the factors behind TB resurgence and measures needed for effective TB control and elimination.
Select the correct answer using the code below
Answer: A
Explanation:
TB's resurgence in the U.S. was due to HIV/AIDS, drug resistance, and immigration from TB-endemic countries. Over-reporting due to enhanced diagnostics was not a reason.
Which of the above statements is/are correct?
Answer: A
Explanation:
Statement 3 is incorrect — TB treatment typically requires 6–9 months, not 10–15 days.
Answer: C
Explanation: The WHO declared TB a global emergency in 1993 primarily due to the dual burden of HIV-TB co-infection and rising drug resistance.
Mains Question: