Maternal Mortality Ratio in India
Syllabus Areas
GS II Governance and Health
93 women lose their life while giving birth in 1 lakh women in India between 2019-21. In other words
“The number of maternal deaths per 100,000 live births during a given time period, usually one year.”
What is Maternal Death?
- The death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
What are Live Births
The total number of births in which the baby shows any sign of life (breathing, heartbeat, umbilical cord pulsation) regardless of gestational age.
Why is it important?
Sustainable Development Goal (SDG) 3: Good Health and Well-Being
Helps track progress toward goals like the SDG Target 3.1:
“Reduce the global maternal mortality ratio to less than 70 per 100,000 live births by 2030.”
MMR in India
| Time Period | MMR (India) |
|---|---|
| 2017–19 | 103 |
| 2018–20 | 97 |
| 2019–21 | 93 |
States have been categorised into three:
- Empowered Action Group (EAG) States
Includes: Bihar, Jharkhand, MP, Chhattisgarh, Odisha, Rajasthan, UP, Uttarakhand, and Assam
- Highest MMR in MP: 175
- Assam: 167
- Other states: Between 100–151
- Jharkhand: 51 (relatively better)
- Southern States
Includes: AP, Telangana, Karnataka, Kerala, Tamil Nadu
- Kerala: 20 (Lowest in India)
- Karnataka: 63 (Highest among southern states)
- Others: 45–49
- Other States
- Maharashtra: 38
- Gujarat: 53
- Punjab: 98
- Haryana: 106
- West Bengal: 109
Challenges:
- Delay in Seeking Care
- Families fail to recognize danger signs during pregnancy or childbirth.
- Social beliefs, lack of awareness, and patriarchal attitudes delay action.
- Financial constraints often prevent timely decision-making.
- ASHAs and ANMs under NRHM have improved institutional delivery rates.
- Incentives to mothers and ASHAs encouraged early care-seeking.
- Delay in Reaching the Facility
- Poor roads and remote locations hinder timely transport.
- Pregnant women often die in transit due to long travel hours.
- 108 ambulance and NHM emergency services have reduced this delay.
- Delay in Receiving Treatment
- Delay in initiating care after reaching the hospital is common.
- Causes include absence of specialists, blood, or OT readiness.
- FRUs were established but face 66% vacancy of specialists.
- Lack of blood banks worsens outcomes in postpartum emergencies.
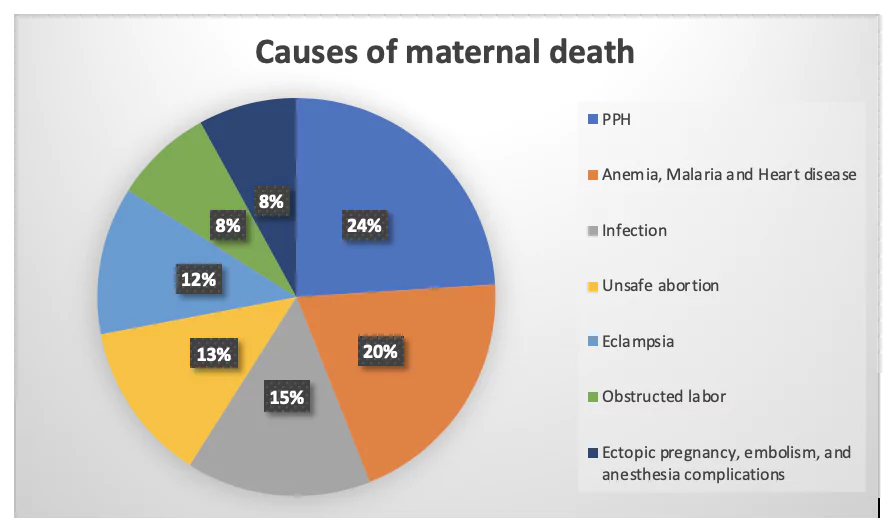
Leading Medical Causes of Maternal Death
- Postpartum Hemorrhage (Bleeding after Delivery)
- Most common cause of maternal death.
- If the uterus doesn’t contract post-delivery, bleeding continues.
- If anaemic, death is faster due to lower blood reserve.
- Requires immediate transfusion and emergency surgery.
- Obstructed Labour
- Seen in young, stunted, underweight mothers.
- Bony pelvis prevents delivery.
- Leads to:
- Uterine rupture.
- Foetal distress.
- Solution: C-section with operation theatre and specialists.
- Hypertensive Disorders (Eclampsia, Preeclampsia)
- Late recognition and treatment leads to:
- Convulsions, coma.
- Death within hours if BP not controlled.
- Late recognition and treatment leads to:
- Infections and Sepsis
- Caused by:
- Unsafe home deliveries.
- Crude abortions by quacks.
- Late hospital admission.
- Caused by:
- Associated Illnesses (especially in EAG States)
- Malaria
- Chronic UTI
- Tuberculosis
→ Increase pregnancy risks significantly.
Best Practices & Kerala Model
- Kerala (MMR = 20) uses:
- Confidential Maternal Death Reviews.
- Technical interventions like:
- Uterine artery clamps.
- Suction cannula.
- Timely management of amniotic embolism, liver failure, DIC.
- Attention to mental health: Managing antenatal/postnatal depression.
Recommended Strategies to Reduce MMR Nationwide
- Ensure early pregnancy registration and comprehensive antenatal check-ups for all women.
- Promote 100% institutional deliveries, especially in EAG States, through ASHA outreach and financial incentives.
- Strengthen and fully staff all First Referral Units, with functional operation theatres, blood banks, and 24x7 specialists.
- Ensure emergency transportation from remote areas using systems like 108 Ambulances.
- Scale up public health nutrition, treat anaemia proactively, and ensure iron-folic acid coverage for all pregnant women.
- Establish mandatory reporting and audits of maternal deaths to improve accountability under the National Health Mission (NHM).
Prelims Questions:
- Consider the following statements regarding the Maternal Mortality
Ratio
(MMR) in India:
- MMR is defined as the number of maternal deaths per 1,00,000 live births.
- The MMR in India has shown a consistent decline from 2017–19 to 2019–21.
- Kerala has the highest MMR among the Southern States.
- Madhya Pradesh reported the highest MMR among all Indian states in 2019–21.
- 1, 2, and 3 only
- 1, 2, and 4 only
- 2, 3, and 4 only
- 1, 3, and 4 only
- Statement 1 is correct.
- Statement 2 is correct (MMR: 103 → 97 → 93).
- Statement 3 is incorrect (Kerala has the lowest MMR = 20).
- Statement 4 is correct (MP has highest MMR = 175).
- Which of the following is/are considered among the "three delays"
model that
contributes to maternal mortality in India?
- Delay in recognising the need for medical care and deciding to seek help
- Delay in receiving care after reaching the health facility
- Delay in transportation from home to hospital
- Delay in childbirth beyond the expected date
- 1, 2, and 3 only
- 1 and 4 only
- 2 and 3 only
- 1, 2, 3, and 4
- Which of the following medical conditions is the leading cause of
maternal death in India as per the data and analysis discussed?
- Eclampsia
- Sepsis
- Postpartum Hemorrhage
- Obstructed Labour
Which of the statements given above are correct?
Answer: B
Explanation:
Answer: A
Explanation:
Delays 1, 2, and 3 are part of Deborah Maine’s "Three Delays Model." Delay 4 is not part of the model.
Answer: C
Explanation:
Postpartum Hemorrhage (severe bleeding after delivery) is the most common and deadliest cause of maternal death in India.